A High Reliability Approach to AI in Healthcare Review
The integration of Artificial Intelligence (AI) into healthcare is rapidly transforming the industry, offering the potential to improve diagnostics, personalize treatment plans, and streamline administrative processes. However, the stakes in healthcare are incredibly high; errors can have life-or-death consequences. This necessitates a high-reliability approach to AI implementation, focusing on safety, accuracy, and transparency. This article will explore the critical aspects of building reliable AI systems for healthcare, examining the challenges and opportunities involved. We’ll delve into specific applications, compare different solutions, and discuss how to ensure that AI enhances, rather than hinders, patient care.
The Imperative of Reliability in Healthcare AI
Imagine a scenario where an AI algorithm misdiagnoses a patient’s condition, leading to incorrect treatment. The consequences could be devastating. This is why reliability isn’t just a desirable feature in healthcare AI; it’s an absolute necessity. The field demands a level of rigor and validation that goes far beyond what might be acceptable in other industries. Think about the difference between an AI recommending a movie you might not like versus an AI recommending the wrong dosage of medication.
Building reliable AI for healthcare requires a multi-faceted approach. It’s not simply about achieving high accuracy on a training dataset. It involves careful consideration of data quality, algorithm selection, explainability, and robust testing. Furthermore, it requires a commitment to continuous monitoring and improvement, as well as a clear understanding of the ethical implications.
The challenge is to harness the power of AI while mitigating the risks. This means developing AI systems that are not only accurate but also transparent, explainable, and resilient to errors. We need to be able to understand how an AI arrived at a particular decision, identify potential biases in the data, and ensure that the system can handle unexpected inputs or scenarios. This is where a high-reliability mindset becomes crucial.
A crucial aspect to consider is the variability of real-world patient data. Datasets used to train AI models are often collected in specific settings and may not accurately reflect the diversity of the patient population. This can lead to biased or inaccurate predictions when the AI is deployed in different environments. Therefore, it is vital to use diverse and representative datasets during training and to continuously monitor the AI’s performance in real-world settings.
Furthermore, the regulatory landscape for healthcare AI is constantly evolving. Healthcare providers and AI developers must stay informed about the latest regulations and guidelines to ensure compliance and to maintain patient safety. Organizations like the FDA are actively working on frameworks for evaluating and approving AI-based medical devices. Adherence to these standards is essential for building trust and ensuring the responsible use of AI in healthcare.
Building Blocks of Reliable AI in Medicine
The foundation of reliable AI in healthcare rests on several key pillars: high-quality data, robust algorithms, explainability, and rigorous validation. Let’s examine each of these components in detail.
Data Quality is Paramount: The adage "garbage in, garbage out" holds especially true in AI. An AI model is only as good as the data it’s trained on. This means ensuring that the data is accurate, complete, and representative of the patient population. Inaccurate or incomplete data can lead to biased or incorrect predictions. Furthermore, it’s crucial to address any potential biases in the data that could perpetuate existing health disparities. For example, if a dataset disproportionately represents one demographic group, the AI model may perform poorly on other groups. Data cleansing and pre-processing are essential steps in building reliable AI models. This includes identifying and correcting errors, handling missing values, and normalizing the data.
Choosing the Right Algorithms: Different AI algorithms are suited for different tasks. Selecting the appropriate algorithm for a specific application is crucial for achieving optimal performance. For example, deep learning models are often used for image recognition tasks, while machine learning algorithms like support vector machines or random forests may be more suitable for predicting patient outcomes. The choice of algorithm should be based on the characteristics of the data, the specific task, and the desired level of explainability. Complex models, like deep neural networks, can be incredibly powerful, but they are often difficult to interpret. Simpler models, like decision trees, may be less accurate but easier to understand.
Explainability is Key: Healthcare professionals need to understand how an AI arrives at a particular decision. This is where explainable AI (XAI) comes in. XAI techniques aim to make AI models more transparent and interpretable. This allows clinicians to understand the reasoning behind an AI’s predictions, which is essential for building trust and ensuring that the AI is used responsibly. There are various XAI techniques available, such as feature importance analysis, which identifies the features that are most influential in the AI’s decision-making process. Explainability is not only crucial for building trust but also for identifying potential biases or errors in the AI model. If a clinician can understand why an AI made a particular prediction, they can better assess its validity and identify any potential flaws.
Rigorous Validation is Essential: Before deploying an AI model in a clinical setting, it’s essential to validate its performance on independent datasets. This involves testing the AI model on data that it hasn’t seen before to assess its ability to generalize to new patients. The validation process should include metrics that are relevant to the clinical application, such as sensitivity, specificity, and accuracy. Furthermore, it’s important to evaluate the AI model’s performance across different demographic groups to ensure that it performs equitably for all patients. Rigorous validation is crucial for identifying any potential weaknesses in the AI model and for ensuring that it meets the required performance standards. This process should also involve clinicians who can assess the AI’s performance from a clinical perspective.
Practical Applications: Where AI Shines in Healthcare
AI is already making a significant impact in various areas of healthcare. Let’s look at some specific examples:
- Diagnostic Imaging: AI can analyze medical images, such as X-rays, CT scans, and MRIs, to detect anomalies and assist radiologists in making diagnoses. For example, AI algorithms can identify subtle signs of cancer that might be missed by human observers.
- Drug Discovery: AI can accelerate the drug discovery process by analyzing vast amounts of data to identify potential drug candidates. This can significantly reduce the time and cost associated with developing new medications.
- Personalized Medicine: AI can analyze patient data, such as genetic information and medical history, to tailor treatment plans to individual patients. This can lead to more effective and personalized care.
- Remote Patient Monitoring: AI can be used to monitor patients remotely, using wearable sensors and other devices. This allows healthcare providers to track patients’ vital signs and detect potential problems early on. For instance, AI-powered systems can monitor elderly patients at home, detecting falls or other emergencies and alerting caregivers.
- Administrative Efficiency: AI can automate administrative tasks, such as scheduling appointments and processing insurance claims. This can free up healthcare professionals to focus on patient care.
Illustrative Scenario: AI in Diabetic Retinopathy Screening
Diabetic retinopathy is a leading cause of blindness in adults. Early detection and treatment are crucial for preventing vision loss. AI algorithms can be used to screen for diabetic retinopathy by analyzing retinal images. These algorithms can identify signs of the disease, such as microaneurysms and hemorrhages, with high accuracy. This allows for early detection and referral to an ophthalmologist for further evaluation and treatment. This is particularly useful in underserved communities where access to ophthalmologists may be limited.
Comparison Table: AI-Powered Diagnostic Imaging Solutions
| Feature | Solution A (Vendor 1) | Solution B (Vendor 2) | Solution C (Vendor 3) |
|---|---|---|---|
| Image Modalities | X-ray, CT | MRI, Ultrasound | X-ray, CT, MRI |
| Target Diseases | Lung Cancer, Pneumonia | Cardiac Disease | Multi-organ screening |
| Accuracy | 95% | 92% | 97% |
| Explainability | Feature Importance | Rule-based reasoning | SHAP values |
| Integration | PACS, EMR | DICOM | Cloud-based |
| Pricing Model | Subscription | Per-image | Enterprise License |
| User Friendliness | High | Medium | Medium |
This table demonstrates the need to consider various factors beyond just accuracy when selecting an AI solution. Integration with existing systems, explainability, and pricing model are all important considerations.
Challenges and Mitigation Strategies
Despite the enormous potential of AI in healthcare, several challenges must be addressed to ensure its safe and effective implementation.
Data Bias: As mentioned earlier, data bias is a significant concern. AI models trained on biased data can perpetuate existing health disparities. To mitigate this risk, it’s crucial to use diverse and representative datasets and to continuously monitor the AI’s performance across different demographic groups. Techniques like adversarial training can also be used to make AI models more robust to bias.
Lack of Explainability: The "black box" nature of some AI models can make it difficult for healthcare professionals to understand how they arrive at their decisions. This can erode trust and make it challenging to identify potential errors. Implementing XAI techniques can help to address this challenge.
Regulatory Hurdles: The regulatory landscape for healthcare AI is still evolving, and there is a lack of clear guidelines and standards. This can create uncertainty for AI developers and healthcare providers. Collaboration between regulatory agencies, AI developers, and healthcare professionals is needed to establish clear and consistent guidelines.
Data Privacy and Security: Protecting patient data is paramount. AI systems must be designed to comply with privacy regulations, such as HIPAA, and to protect against data breaches. Encryption, access controls, and data anonymization techniques are essential for ensuring data privacy and security.
Clinician Acceptance: Some healthcare professionals may be hesitant to adopt AI, due to concerns about job displacement, lack of trust, or difficulty understanding the technology. It’s crucial to involve clinicians in the development and implementation of AI systems and to provide them with adequate training and support. Demonstrating the benefits of AI and addressing their concerns can help to foster greater acceptance.
Continuous Monitoring and Improvement: AI models are not static; their performance can degrade over time due to changes in the patient population or the environment. It’s essential to continuously monitor the AI’s performance and to retrain it as needed. This requires establishing a robust monitoring system and having a process in place for updating the AI model.
The Future of AI in Healthcare: A Collaborative Approach
The future of AI in healthcare is bright, but it requires a collaborative approach. AI developers, healthcare professionals, regulatory agencies, and patients must work together to ensure that AI is used safely, ethically, and effectively.
AI should be viewed as a tool to augment human capabilities, not to replace them. Healthcare professionals will continue to play a crucial role in patient care, using AI to assist them in making better decisions. The focus should be on developing AI systems that are user-friendly, explainable, and aligned with clinical workflows.
The use of federated learning, where AI models are trained on decentralized data sources, can help to address data privacy concerns and to improve the generalizability of AI models. Federated learning allows AI models to be trained on data without sharing the data itself, which can be particularly useful in healthcare, where data privacy is paramount.
Furthermore, the development of AI standards and certifications can help to ensure the quality and reliability of AI systems. This will help to build trust and to promote the responsible use of AI in healthcare. Organizations like the FDA and the IEEE are actively working on developing these standards.
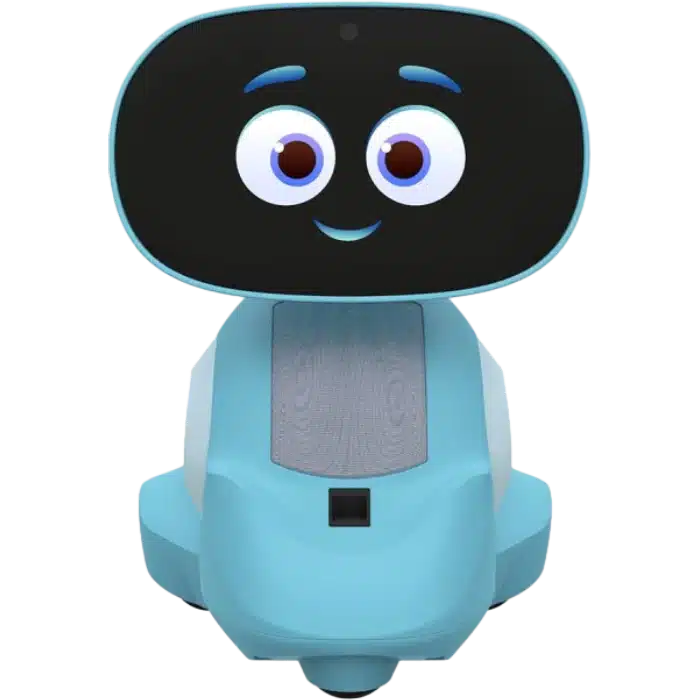
AI robots are also making headway in healthcare, assisting with tasks such as medication dispensing, patient transport, and even surgery. AI Robots for Home, while not directly applicable in the same hospital context, share similar underlying technologies of navigation and task execution. Understanding these core AI components is essential for any successful deployment in medical settings.
The ultimate goal is to create a healthcare system that is more efficient, personalized, and accessible to all. AI has the potential to help us achieve this goal, but only if we approach its implementation with a high-reliability mindset and a commitment to patient safety and well-being.
FAQ: AI in Healthcare
Q: How can I ensure the data used to train AI models in healthcare is unbiased?
A: Ensuring unbiased data for AI models in healthcare is crucial for equitable outcomes. Begin by collecting data from diverse sources representing the full spectrum of the patient population, including various demographics, socioeconomic backgrounds, and geographic locations. Scrutinize the data collection process for potential biases introduced during data entry, labeling, or sampling. Implement data augmentation techniques to balance underrepresented groups and mitigate bias. Regularly audit the trained AI model’s performance across different subgroups to identify and correct any disparities. Moreover, involve diverse teams in the development and validation process to bring different perspectives and identify potential biases that might be overlooked. Employing bias detection tools and algorithms can further aid in identifying and mitigating bias in the data and model. Continuously monitor and evaluate the AI model’s performance in real-world settings to ensure fairness and prevent the perpetuation of health disparities.
Q: What are the key ethical considerations when using AI in healthcare?
A: Key ethical considerations in using AI in healthcare revolve around patient autonomy, privacy, fairness, and transparency. Patient autonomy must be respected by ensuring that individuals are informed about the use of AI in their care and have the right to refuse AI-driven interventions. Patient privacy is paramount, requiring robust data security measures and compliance with regulations like HIPAA to protect sensitive health information. Fairness necessitates mitigating biases in AI algorithms to prevent discriminatory outcomes and ensure equitable access to quality care for all patients, regardless of demographic factors. Transparency is essential to build trust and allow healthcare professionals to understand how AI models arrive at decisions, facilitating accountability and enabling appropriate oversight. Additionally, the potential for job displacement among healthcare workers due to AI automation requires proactive planning and workforce retraining initiatives. Striking a balance between leveraging the benefits of AI and upholding ethical principles is crucial for responsible AI implementation in healthcare.
Q: How can healthcare professionals be trained to effectively use AI tools in their practice?
A: Training healthcare professionals to effectively use AI tools requires a comprehensive and multifaceted approach. Begin by providing foundational education on AI concepts, machine learning, and data science principles relevant to their specific roles and clinical areas. Offer hands-on training sessions using real-world case studies and practical exercises to familiarize them with AI tools and their applications in diagnostics, treatment planning, and patient management. Incorporate AI training into medical school curricula, residency programs, and continuing medical education (CME) courses to ensure ongoing learning and skill development. Emphasize the importance of critical thinking and clinical judgment when interpreting AI-generated insights, reminding them that AI is a tool to augment, not replace, their expertise. Provide access to AI experts and technical support to address questions and troubleshoot issues as they arise. Foster a culture of collaboration and knowledge sharing among healthcare professionals to promote best practices and accelerate AI adoption. Regularly update training programs to reflect the latest advancements in AI technology and clinical guidelines.
Q: What is the role of regulatory bodies like the FDA in overseeing the use of AI in healthcare?
A: Regulatory bodies like the FDA play a crucial role in overseeing the use of AI in healthcare to ensure patient safety, efficacy, and reliability. The FDA’s oversight involves evaluating the safety and effectiveness of AI-based medical devices and software through rigorous pre-market review processes. This includes assessing the AI algorithm’s performance, evaluating its ability to produce accurate and consistent results, and ensuring that it meets established standards for medical devices. The FDA also monitors AI-based medical devices post-market to identify and address any safety concerns or performance issues that may arise after they are deployed in clinical settings. Establishing clear guidelines and standards for the development, validation, and deployment of AI in healthcare is also part of the FDA’s role. This provides manufacturers with a framework for developing safe and effective AI-based medical devices and ensures that healthcare professionals can trust the reliability of these technologies. Collaboration with stakeholders, including AI developers, healthcare providers, and patients, is also critical to stay informed about emerging trends and challenges in AI healthcare.
Q: What are the limitations of current AI technology in healthcare?
A: Current AI technology in healthcare, while promising, faces several limitations. Data bias is a significant concern, as AI models trained on biased datasets can perpetuate and amplify existing health disparities. Limited explainability of complex AI models, often referred to as "black boxes," makes it difficult for healthcare professionals to understand the reasoning behind AI-driven recommendations, hindering trust and adoption. The lack of standardized data formats and interoperability between different healthcare systems poses challenges for seamless integration of AI tools into clinical workflows. The need for large, high-quality datasets for training AI models can be a barrier, particularly for rare diseases or specialized areas of medicine. Regulatory and ethical frameworks for AI in healthcare are still evolving, creating uncertainty and potentially slowing down innovation. Finally, the risk of overfitting, where AI models perform well on training data but poorly on new data, necessitates rigorous validation and monitoring.
Q: How can AI be used to improve access to healthcare in underserved communities?
A: AI can significantly improve access to healthcare in underserved communities through several avenues. Telehealth platforms powered by AI can provide remote consultations, diagnosis, and monitoring, overcoming geographical barriers and reducing the need for travel. AI-powered chatbots and virtual assistants can offer basic medical information, triage patients, and schedule appointments, reducing the burden on limited healthcare resources. AI algorithms can analyze medical images, such as X-rays and CT scans, to detect diseases early, enabling timely intervention and preventing complications. Personalized treatment plans generated by AI can optimize resource allocation and improve patient outcomes, especially in areas with limited access to specialized care. Predictive analytics powered by AI can identify individuals at high risk of developing certain conditions, allowing for proactive interventions and preventive care. Language translation tools driven by AI can facilitate communication between healthcare providers and patients who speak different languages, ensuring equitable access to care.

Price: $56.99 - $43.47
(as of Sep 04, 2025 18:52:25 UTC – Details)
All trademarks, product names, and brand logos belong to their respective owners. didiar.com is an independent platform providing reviews, comparisons, and recommendations. We are not affiliated with or endorsed by any of these brands, and we do not handle product sales or fulfillment.
Some content on didiar.com may be sponsored or created in partnership with brands. Sponsored content is clearly labeled as such to distinguish it from our independent reviews and recommendations.
For more details, see our Terms and Conditions.
:AI Robot Tech Hub » A High Reliability Approach to AI in Review AI In Healthcare – Didiar
 AI Robot Tech Hub
AI Robot Tech Hub